Cerebral Palsy and Music
Wear green to support World Cerebral Palsy Day! October 6th is World Cerebral Palsy (CP) Day - a day aimed at bringing together people living with cerebral palsy, their families, and supporters all over the world. To celebrate World CP Day, we wanted to share a little bit about how neurologic music therapy® can be beneficial for those living with CP.
Music Heals: How Music Saves Us
Many of us have a favorite song we turn to when we’re feeling sad, depressed, anxious, and feel like we have nowhere else to go. This song or this artist is our solace, our refuge, and a place we call home. When the world seems cold and cruel, our favorite music is like a cozy fireplace that keeps us warm and makes us feel safe. Although this is not exactly music therapy, there is a common saying- “When words fail, music speaks.”
More Than ‘Man’s Best Friend’
For some of our clients at Perfect Harmony Health, having access to service dogs can help make a difference in their everyday lives. I had the pleasure of interviewing McKenzie Wortman, diagnosed with Cerebral Palsy who receives Neurologic Music Therapy (NMT)® services at Perfect Harmony Health, and Tricia Simonds, a parent within our community, to help us understand the benefits of service dogs, the process of receiving service dogs, what populations service dogs can serve and how they serve them, the process of how they are trained, and their personal experiences with their own service dogs.
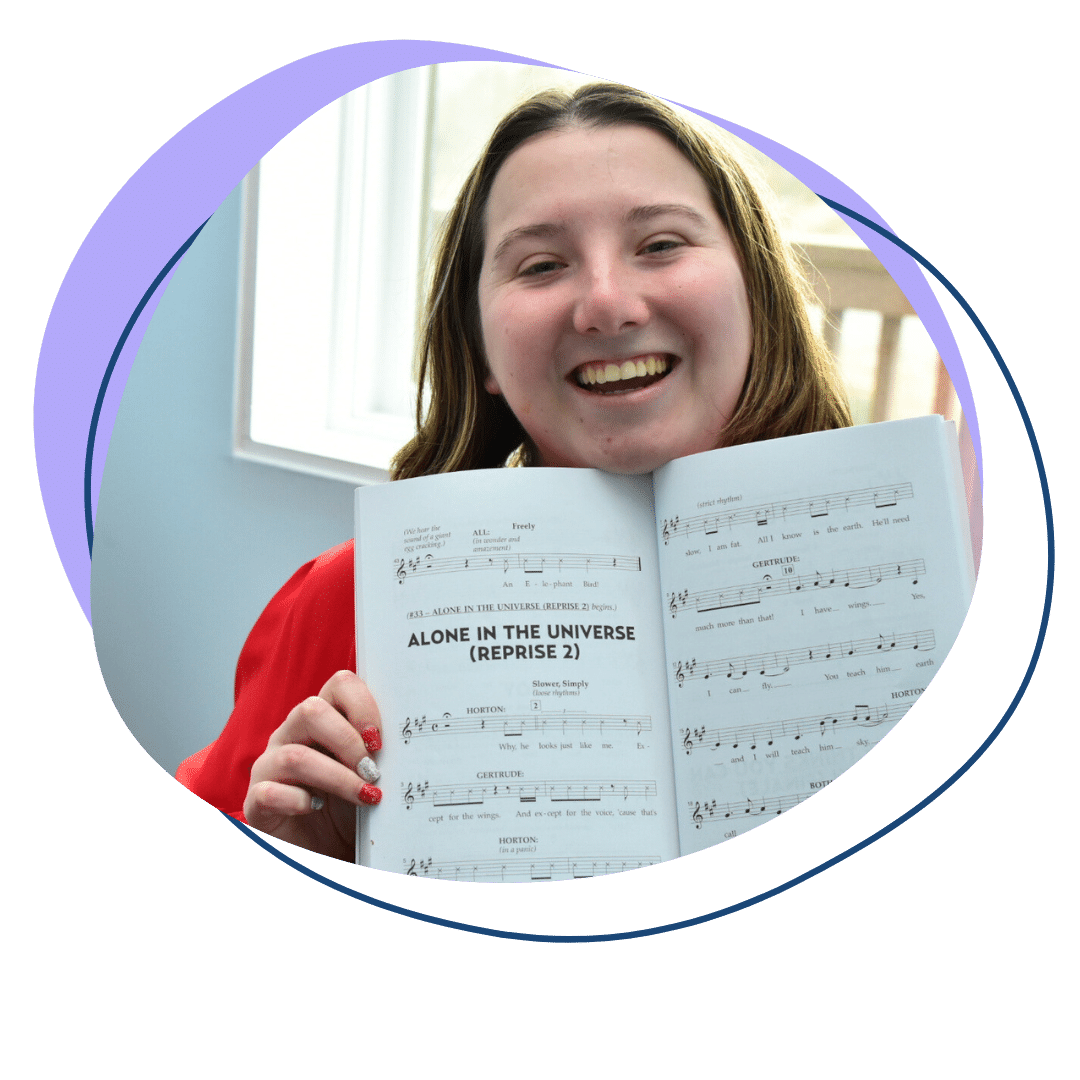
Inclusive Theatre: Roswell Players
Every Fall, schools around Georgia begin their theatre program rehearsals. Unfortunately, not many of those programs are available to welcome teens or adults with neurodivergent, learning or physical difficulties. That is where Roswell Players at Perfect Harmony Health comes in!